Glaucoma is one of the most common eye conditions and causes the optic nerve to deteriorate due to abnormally increased eye pressure gradually. The optic nerve is in charge of sending visual information from your eye to your brain.
When the different types of glaucoma affect the eye, fluid starts to build up in the front part of the eye, causing blind spots in the vision.
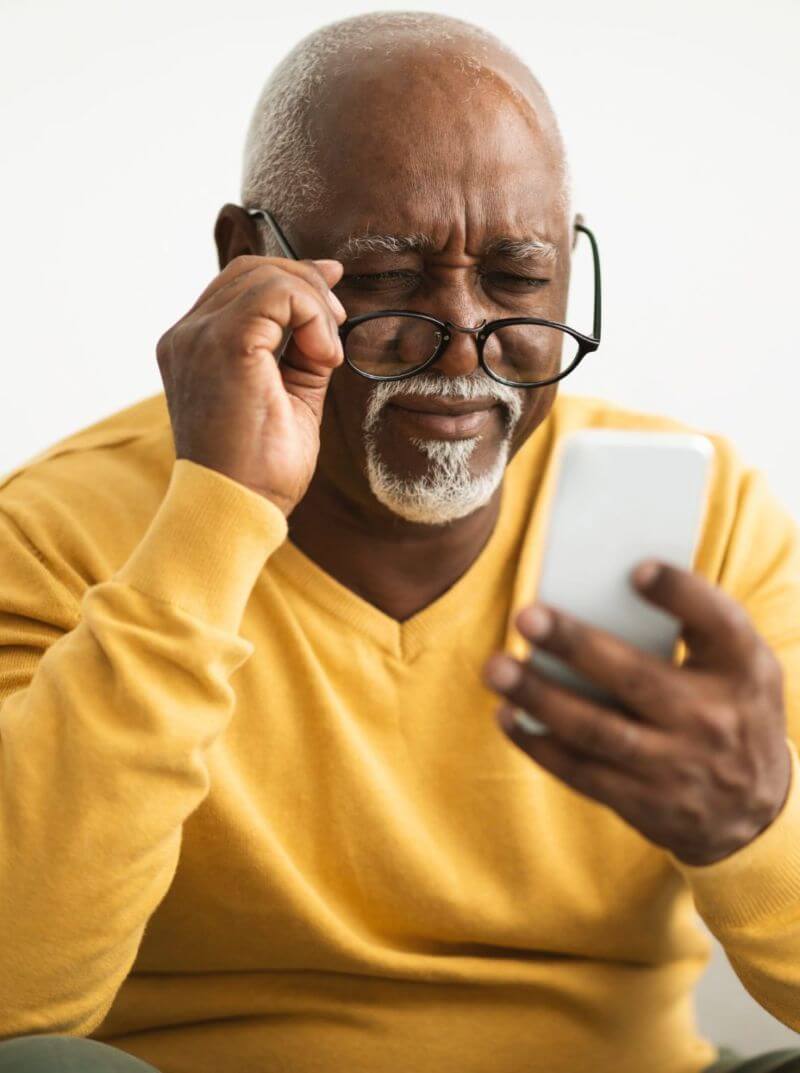
In the early stages of glaucoma, there may be no noticeable signs. However, as the condition advances, symptoms may include a gradual loss of vision, blurred vision, halos around lights, and difficulty seeing in low light. In severe cases, undiagnosed and untreated, glaucoma can lead to vision loss.
Regular eye exams are the best way to identify glaucoma in the earliest stages. Treatment may include prescription eye drops to lower intraocular pressure, laser therapy, or surgery.
There are different types of glaucoma, including:
If left untreated, glaucoma can damage the optic nerve to the point of blindness. Some of the risk factors associated with it involve:
Glaucoma can develop gradually without any noticeable symptoms during its early stages. As it progresses, symptoms may start to appear. These include:
Glaucoma is diagnosed through a comprehensive eye exam, which typically includes:
Based on the results of these tests and evaluations, your doctor will determine if you have glaucoma and the type and severity of the condition.
Treatment for glaucoma and other optic nerve problems usually involves lowering the intraocular pressure that damages the optic nerve or draining excess fluid from the eye.
This can be achieved with eye drops, medication, laser treatment, surgery, or a combination of these. Choosing the right procedure will depend on your specific needs and the extent of damage in your eyes.
Eye drops to treat glaucoma work by reducing the pressure inside the eye. The most common type of eye drops include the following:
When eye drops do not help decrease intraocular pressure completely, your doctor may recommend using prescription medication to inhibit the production of eye fluids.
In case your doctor determines it is not the right procedure for you, laser treatment can help improve eye fluid drainage. With laser treatment, the angle where the iris and cornea meet will open up, allowing intraocular pressure to lower.
Depending on the complexity of your case, your doctor may recommend glaucoma surgery as the last resource. During your surgery, the following steps will take place:
You will need to rest for a few days after surgery, avoiding certain physical activities. However, full recovery may take several months. Your doctor may prescribe eye drops and will suggest you attend follow-up appointments to monitor your case.
Glaucoma is a life-long condition that has no cure. However, several lifestyle changes can help you manage its symptoms; these include:
EyesNY offers treatment to help patients dealing with glaucoma and other optic nerve problems. Our specialized team of ophthalmologists is ready to assess your needs and give you the high-quality vision care you deserve.
We work with cutting-edge technology to identify the root cause of your condition and create personalized treatment plans. Our caring staff is ready to welcome you and meet your ocular health and vision needs.
We offer comprehensive eye care services, including treatment for glaucoma and other types of optic nerve problems.
If you’d like a consultation or more information, contact us, request an appointment online, or visit our clinics. We have multiple locations around New York, including Malta, Clifton Park, Troy, Saratoga Springs, and Queensbury.
Malta
658 Malta Ave., Ste 101
Malta, NY 12020
Phone: (518) 580-0553
Saratoga Springs
414 Maple Ave Ste 200
Saratoga Springs, NY 12866
Phone: (518) 580-0553
Clifton Park
1712 U.S. 9
Clifton Park, NY 12065
Phone: (518) 580-0553
Queensbury
535 Bay Road
Queensbury, NY 12804
Phone: (518) 580-0553
Troy
2200 Burdett Street Ste 206
Troy, NY 12180
Phone: (518) 580-0553
